Vol. 4 (2024), Article ID 246169, 5 pages
Research Article
Impact of New Criteria for Gonadotoxic Risk Stratification on an Oncology Population in a Pediatric Hospital
Alejandra Dumenigo,1,2 Olivia Frias,2 Karen Burns,1,2 Julie Rios3
1College of Medicine, University of Cincinnati, Cincinnati, OH 45229, USA
2Cincinnati Children’s Hospital Medical Center, Cincinnati, OH 45229, USA
3School of Medicine, University of Pittsburgh, Pittsburgh 15261, PA, USA
Received 9 January 2024; Revised 19 November 2024; Accepted 23 November 2024; Published 18 December 2024
Alejandra Dumenigo, Olivia Frias, Karen Burns, Julie Rios, Impact of New Criteria for Gonadotoxic Risk Stratification on an Oncology Population in a Pediatric Hospital, Journal of Fertility Preservation, 4 (2024), art246169. doi:10.32371/jfp/246169
Background. In 2020, new criteria were published for gonadotoxic risk stratification in pediatric patients receiving chemotherapy or radiation. The changes may impact fertility preservation (FP) counseling as some options for FP are experimental and only offered to those with high-risk stratification under current IRB protocols. Purpose. We describe the population affected by the change in criteria and how it impacted FP counseling. Methods. 241 charts within the Cincinnati Children’s Hospital Medical Center (CCHMC) fertility registry were reviewed for gonadotoxic treatment dosing at the time of FP consultation. Risk assessments were completed with the new criteria. Descriptive statistics were used to analyze data. Results. Of 241 patients, 5.4% (n = 13) had a change in risk stratification. Six patients would have been eligible for an experimental FP option by the new criteria. More of the eligible patients were male, had lymphoma, and had a risk change from intermediate to high risk (Table 1). Conclusion. Very few patients had a change in risk that affected FP options. Demographics and diagnosis were not homogenous but male patients and those with lymphoma were affected most.
risk stratification; gonadotoxic; CED; fertility preservation; gonadal insufficiency
Advancements in treatment and increased survival rates for pediatric and adolescent cancer have allowed for an increased focus on the long-term effects associated with these treatments. Due to exposure to potentially gonadotoxic therapies, gonadal insufficiency is one of many long-term effects of treatment known to cause psychosocial issues and distress among survivors [1]. Research has shown that these stressors can be alleviated through access to fertility counseling and fertility preservation (FP) before treatment. Despite the stress and time constraints of initiating treatment as well as the experimental nature of some FP options, patients are interested in receiving fertility counseling and when they do, they report greater satisfaction and less decisional regret regardless of whether they ultimately pursue the FP [2].
Within the relatively new world of pediatric oncofertility, FP options for post-pubertal female sex include oocyte and embryo cryopreservation, ovarian transposition, and shielding from radiation. Post-pubertal male sex FP options include sperm cryopreservation, testicular sperm extraction, and gonadal shielding. For pre-pubertal individuals and for those who cannot delay life-saving therapy, ovarian tissue cryopreservation (OTC) for female and testicular tissue cryopreservation (TTC) for male patients are alternatives [2]. In 2020, the American Society of Reproductive Medicine released guidelines stating OTC is no longer experimental. Therefore, counseling around OTC should reflect this recent change as the standard of care for female patients who qualify; however, there is limited data in pediatric populations. TTC remains an experimental study for prepubertal patients as well as adolescent and young adult males under 25 years of age who are unable to provide a sperm specimen [3].
Oncofertility risk assessment tools created by the Pediatric Initiative Network (PIN) allow for the stratification of patients based on treatment regimen and clinical factors so that medical care providers and patients may select the appropriate method of FP when indicated. In 2020, the PIN developed the first pediatric and adolescent and young adult-specific gonadotoxic risk stratification guidelines to call for the most accurate pre-gonadotoxic treatment counseling. Known gonadotoxic risk is based on cancer therapy and general guidelines, placing the male and female patients into one of the following three categories: highly increased risk, significantly increased risk, or minimally increased risk (Figures 1 and 2) [4]. Previous adult-based stratification guidelines—extrapolated for pediatric use—utilized three categories: high risk, intermediate risk, or low risk [5].

Figure 1: Risk stratification grid—male sex [
4].
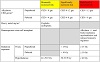
Figure 2: Risk stratification grid—female sex [
4].
Doses and types of chemotherapeutic agents, as well as doses of pelvic radiation, are currently utilized to risk stratify patients [5,6]. Age at time of diagnosis or therapy administration also influences this assessment [4,6]. The gonadotoxicity of treatment is drug- and dose-dependent and to quantify cumulative exposure to the chemotherapeutic alkylating agents across protocols, Cyclophosphamide Equivalent Dose (CED) is used [7]. Doses of alkylating agents including cyclophosphamide, ifosfamide, procarbazine, chlorambucil, BCNU (carmustine), CCNU (lomustine), melphalan, Thio-TEPA, nitrogen mustard, and busulfan are considered in the calculation. A CED of ≥8,000 gm/m2 and 4,000 gm/m2 in prepubertal and pubertal
female patients respectively is considered gonadotoxic. In all patients of male sex, a CED of ≥4,000 gm/m2 is considered gonadotoxic [4]. The most notable change in risk stratification categories with this new model saw the male sex risk stratification table go from three categories to two when using CED for alkylating agents. In addition to the CED, exposure to cisplatin and carboplatin is considered to increase risk. Lastly, bone marrow transplantation (hematopoietic stem cell transplantation) increases risk due to agents (ex. cyclophosphamide, busulfan, or melphalan) used in conditioning for the myeloablation process [2].
Since the change in the guidelines, no data have been published describing which populations or diseases may have been affected by these updates. The purpose of this study was to use the Cincinnati Children’s Hospital and Medical Center’s (CCHMC) Comprehensive Fertility Care and Preservation Program (CFCPP) patient database to determine which populations, cancer types, and treatment modalities were impacted by the change in risk stratification. This information can later be applied during survivorship care to better counsel patients regarding future fertility status. We hypothesized that only a small portion of patients would have been counseled differently based on new criteria and that those of male sex would be affected more than female sex since the male sex risk stratification system now used two categories as opposed to three.
At CCHMC, patients facing potentially gonadotoxic therapy could receive a consultation with the CFCPP team before starting therapy at the institution if no exclusion criteria were met. Prior to the FP consultation, a fertility risk assessment was completed by a pediatric oncologist based on the proposed treatment regimen. Patients were stratified as being at low, intermediate, or high risk of gonadotoxicity based on age/pubertal status, chemotherapy and/or total body radiation dose, and other patient and treatment factors. FP consultations were then conducted with gynecology or urology teams to discuss gonadal insufficiency risk and FP treatment options. Patients who received an FP consultation were added to the CFCPP Fertility Care and Research Registry, which included patient demographics, oncologic diagnosis, intended therapy, gonadotoxic risk assessment score, and FP treatments.
Following IRB approval, we reviewed subjects within the CCHMC fertility registry from 2014 to 2020. Eligible patients (510 total) included those who had been designated a gonadotoxic risk assessment group based on prior criteria and had received a prior fertility consultation based on this designation. Patients were excluded if the initial risk assessment was categorized as high, as their eligibility for FP would not have been impacted by new criteria. Additionally, patients who had received prior cancer treatment at an outside facility were excluded since total CED could not be determined. After exclusion, 241 charts were reviewed for gonadotoxic treatment dosing at the time of the fertility consultation. Using the new criteria, we then completed risk assessments based on the CED dosing available at the time of the initial consultation.
Descriptive statistics were used to compare patients with a change in risk of gonadotoxicity based on the new criteria to patients who did not have a change in risk category. Demographics such as pubertal status, CED dosing, type of cancer, sex, and age were compared among groups. The Wilcoxon Sum Rank test for continuous variables and Chi-Square or Fischer’s exact test for categorical variables were used given small sample size affecting normal distribution. All tests employ a two-tailed, α = 0.05, unadjusted for multiple tests.
Of the 241 patients included in the study, only 5.4% (n = 13) had a change in the risk assessment. No patients had a reduction in risk assessment from the initial consultation. The risk assessment of 3 patients changed from minimally increased risk to significantly increased risk. The risk assessment of 7 patients changed from significantly
increased risk to high level of increased risk. The risk assessment of 3 patients changed from minimally increased risk to high level of increased risk. Of these 13 patients, 9 were male. Five male patients had a diagnosis of lymphoma, 2 osteosarcoma, 1 neuroblastoma, and 1 relapsed acute lymphocytic leukemia (ALL). The remaining 4 female patients included 1 neuroblastoma, 1 T cell lymphoma, 1 rhabdomyosarcoma, and 1 osteosarcoma diagnosis.
As a result of a change to the risk assessment, 6 of these 13 patients would now qualify for the FP protocols that they did not meet the criteria for prior treatment. Specifically, 1 female patient and 5 male patients would have been appropriate to consider for OTC and TTC respectively. Of the remaining 7 of 13, 2 completed and 5 declined the FP option prior to treatment. Patient demographics are represented in Table 1.

Table 1: Patients affected by change in risk stratification.
Our study found a small percentage of patients would have had a different risk assessment based on the new criteria. The groups most affected by these changes were male patients and individuals with lymphoma. Among those with lymphoma, the majority were male. As previously mentioned, the stratification for male patients changed from three categories to two categories, resulting in more patients falling into the high risk category now that the intermediate risk category was eliminated. Patients who receive standard lymphoma therapy protocols are more likely to receive a CED that was affected by this change. Minimal patients had an increase in risk assessment which may have affected eligibility for certain FP procedures.
Of the FP procedures, OTC has been shown to be safe and effective in all ages [2], but still there is no consensus on who qualifies to receive the therapy. This is likely due to multi-disciplinary collaboration and various ethical concerns that come with the procedures. TTC has also been found to be safe, but being that it is still an experimental procedure, eligibility varies depending on the investigational protocol [2]. The Edinburg Criteria remain a commonly used guide for determining the eligibility of patients for OTC and TTC [8]. For OTC, the criteria are as follows: age younger than 35 years; no previous chemotherapy or radiotherapy if 15 years or older at diagnosis with mild non-gonadotoxic chemotherapy acceptable if younger than 15 years; realistic chance of surviving for 5 years; high risk of premature ovarian insufficiency (>50%); informed consent (from parents and, where possible, the patient); negative serology results for HIV, syphilis, and hepatitis B; not pregnant and no existing children. Similar Edinburg criteria exist for TTC including age 0–16 years; high risk of infertility (>80%); unable to produce a semen sample by masturbation; no clinically significant pre-existing testicular disease (e.g., cryptorchidism); and same informed consent and negative serology as female patients. One study reported that these criteria are too restrictive, based on the success of OTT [9]. However, a recent study by Duffin et al. [10] in female patients found the Edinburgh criteria to be a robust tool in predicting ovarian insufficiency prior to gonadotoxic treatment although the study was limited by some loss to follow-up. Further long-term studies are needed as well as studies in male patients to understand whether these criteria are too strict, leading to unnecessary preservation of gonadal tissues.
Our study serves as the first of its nature to determine the impact of the first pediatric and adolescent and young adult-specific gonadotoxic risk stratification guidelines on an oncology population in a pediatric hospital; however, the data that exists suggests that having an increased risk assessment would have increased the likelihood of these patients pursuing FP options [10]. Other predictors for pursuing FP include male sex, increased age, increased developmental status, and not being from the United States. This is encouraging data since as we hypothesized, more male sex patients were affected by the increase in fertility risk. Conflicting results exist regarding whether
race, ethnicity, primary language, or insurance status predict the likelihood of choosing to pursue FP [11,12,13]. Notably, populations with worse prognosis, advanced
disease, advanced reproductive age, prior parity, and those identifying as LGBTQ have been found to experience more provider bias and have decreased access to FP services, to begin with [13,14,15]. This is especially concerning since older patients are at an increased risk of gonadotoxicity from these treatments. Future studies should continue to evaluate how patient demographics influence shared decision-making in FP.
In addition to lack of access, a lack of shared decision-making continues to be associated with decreased patient satisfaction rates with their oncofertility treatment despite an increased emphasis on the shared decision-making model in medicine at large [16]. Aspects of a shared decision model including “active listening; open, honest, non-judgmental communication; in an environment that promoted respect; empowered women to discuss personal thoughts and emotions; trustworthiness; alongside efforts to decrease stress or tension” [15] as well as the use of patient decision aids [16] have been found to improve these outcomes and should also be considered when discussing FP with patients.
This study has many strengths, including the large, diverse patient population with multiple diagnoses. Limitations of the study include the nature of a retrospective review which may allow for errors in data analysis. Additionally, because this is a retrospective study, we had to exclude patients with prior treatment at outside hospitals since detailed information was not always available to calculate the CED rate. Lastly, the CED rate itself is not prognostic. Although increasing CED correlates with an increased risk of gonadotoxicity, minimum exposure to alkylating agents still carries a risk of gonadotoxicity [7,17]. Similarly, CED causing “high level of increased risk” does not always cause gonadal insufficiency. Therefore, it is crucial that patients and their families receive thorough education regarding the risk of gonadal insufficiency from exposure to gonadotoxic therapies to ensure informed consent.
By better characterizing fertility risk assessment under the new criteria, patients and families can be better informed in making decisions on FP. To provide the best care for patients, survivorship providers should be aware of changes in stratification and individualize counseling by total CED received at the time of treatment. If necessary, post-treatment patients can be made aware of these changes during routine follow-up survivor care visits and offered an additional fertility consultation. The next steps in evaluating the impact of these risk stratification changes involve assessing the psychosocial effects on patients and families, as well as examining how the revised information may have influenced decisions regarding fertility preservation.
While there have been great advances in understanding the gonadotoxic risk for pediatric patients receiving chemotherapy or radiation, risk stratification continues to evolve, thereby enhancing our FP counseling. In this study, very few patients experienced a change in risk stratification that impacted FP options. Demographics and diagnosis were not homogenous, but male patients and those with lymphoma were affected the most under the new criteria. This paper identifies a population that survivorship providers should be aware of as the most affected by the
criteria in order to provide appropriate FP counseling.
| ALL: | Acute lymphocytic leukemia |
| CCHMC: | Cincinnati Children’s Hospital Medical Center |
| CED: | Cyclophosphamide equivalent dosing |
| CFCPP: | Comprehensive Fertility Care and Preservation Program |
| FP: | Fertility preservation |
| OTC: | Ovarian tissue cryopreservation |
| PIN: | Pediatric initiative network |
| TTC: | Testicular tissue cryopreservation |
| |
| |
| |
The authors thank Dr. Lesley Breech, Brycen Ferrah, and providers within the Gynecology, Urology, and Oncology Departments of CCHMC for their collaboration and support in developing the CFCPP Fertility Care and Research Registry.
The authors declare that they have no conflict of interest.
- S. Logan, J. Perz, J. M. Ussher, M. Peate, and A. Anazodo, Systematic review of fertility-related psychological distress in cancer patients: Informing on an improved model of care, Psychooncology, 28 (2019), 22–30.
- K. C. Burns, H. Hoefgen, A. Strine, and R. Dasgupta, Fertility preservation options in pediatric and adolescent patients with cancer, Cancer, 124 (2018), 1867–1876.
- L. Nahata, T. K. Woodruff, G. P. Quinn, et al., Ovarian tissue cryopreservation as standard of care: what does this mean for pediatric populations?, J Assist Reprod Genet, 37 (2020), 1323–1326.
- L. R. Meacham, K. Burns, K. E. Orwig, and J. Levine, Standardizing risk assessment for treatment-related gonadal insufficiency and infertility in childhood adolescent and young adult cancer: The pediatric initiative network risk stratification system, J Adolesc Young Adult Oncol, 9 (2020), 662–666.
- C. L. Nieman, K. E. Kinahan, S. E. Yount, et al., Fertility preservation and adolescent cancer patients: lessons from adult survivors of childhood cancer and their parents, Cancer Treat Res, 138 (2007), 201–217.
- E. J. Chow, K. L. Stratton, W. M. Leisenring, et al., Pregnancy after chemotherapy in male and female survivors of childhood cancer treated between 1970 and 1999: a report from the Childhood Cancer Survivor Study cohort, Lancet Oncol, 17 (2016), 567–576.
- D. M. Green, V. G. Nolan, P. J. Goodman, et al., The cyclophosphamide equivalent dose as an approach for quantifying alkylating agent exposure: a report from the Childhood Cancer Survivor Study, Pediatr Blood Cancer, 61 (2014), 53–67.
- R. A. Anderson, R. T. Mitchell, T. W. Kelsey, N. Spears, E. E. Telfer, and W. H. Wallace, Cancer treatment and gonadal function: experimental and established strategies for fertility preservation in children and young adults, Lancet Diabetes Endocrinol, 3 (2015), 556–567.
- D. Meirow, H. Ra’anani, M. Shapira, et al., Transplantations of frozen-thawed ovarian tissue demonstrate high reproductive performance and the need to revise restrictive criteria, Fertil Steril, 106 (2016), 467–474.
- K. Duffin, R. Howie, T. W. Kelsey, H. B. Wallace, and R. A. Anderson, Long-term follow-up to assess criteria for ovarian tissue cryopreservation for fertility preservation in young women and girls with cancer, Hum Reprod, 38 (2023), 1076–1085.
- M. R. Sax, G. Pettengill, A. Hasija, et al., Factors associated with fertility preservation in a pediatric, adolescent and young adult population, J Pediatr Hematol Oncol, 44 (2022), 369–375.
- D. M. Flink, J. Sheeder, and L. A. Kondapalli, Do patient characteristics decide if young adult cancer patients undergo fertility preservation?, J Adolesc Young Adult Oncol, 6 (2017), 223–228.
- L. Coker Appiah, Y. F. Fei, M. Olsen, S. R. Lindheim, and D. M. Puccetti, Disparities in female pediatric, adolescent and young adult oncofertility: A needs assessment, Cancers (Basel), 13 (2021), 5419.
- A. Korkidakis, K. Lajkosz, M. Green, D. Strobino, and M. P. Velez, Patterns of referral for fertility preservation among female adolescents and young adults with breast cancer: A population-based study, J Adolesc Young Adult Oncol, 8 (2019), 197–204; erratum in: J Adolesc Young Adult Oncol, 9 (2020), 546–547.
- S. Logan, J. Perz, J. M. Ussher, M. Peate, and A. Anazodo, A systematic review of patient oncofertility support needs in reproductive cancer patients aged 14 to 45 years of age, Psychooncology, 27 (2018), 401–409.
- G. Jones, J. Hughes, N. Mahmoodi, E. Smith, J. Skull, and W. Ledger, What factors hinder the decision-making process for women with cancer and contemplating fertility preservation treatment?, Hum Reprod Update, 23 (2017), 433–457.
- D. M. Green, W. Liu, W. H. Kutteh, et al., Cumulative alkylating agent exposure and semen parameters in adult survivors of childhood cancer: a report from the St Jude Lifetime Cohort Study, Lancet Oncol, 15 (2014), 1215–1223.
Copyright © 2024 Alejandra Dumenigo et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.